How Does Hospital Billing Work: Avoid Common Errors Now

Hospital bills can be complex and confusing, but How Does Hospital Billing Work? It's also a time-consuming and challenging procedure. When a person is accepted into a medical facility, their primary concern is their health, not their monetary expenditures.
Obtaining knowledge regarding the inner workings of hospital bills may reduce some of the anxiety and worry associated with hospital bills.
In this article, we'll tour how hospital bills work. From the initial charge capture to the final payment by insurance companies or patients.
What Is Hospital Billing?
Hospital billing is the process of collecting fees for medical services. Hospital billing is an indispensable part of the healthcare industry. It involves the delicate submission and processing of insurance claims for medical services rendered to patients.
Hospital billing involves several keys player, including healthcare providers, insurance providers, and patients.
This complex process demands accuracy, precision, and meticulous attention to detail as it surrounds collecting and authenticating Patient information.
The coding of medical procedures and diagnoses, the submission of claims to insurance providers, and the pursuit of claims rejected or denied for various reasons.
Types Of Hospital Billing?
Hospital health facilities do not use only one medical billing system. Hospital billing is vital in ensuring that the provider receives timely reimbursement for the rendered services, optimising their revenue cycle performance. Let's discover the different types of hospital billing systems and who are the users of those systems and how hospital billing works.
i) Closed Medical Billing System
As the name suggests, a 'closed' medical billing system means that the billing charts and associated health records remain within the boundaries of a particular clinician. Electronic Medical Record (EMR) is the most common digital tool for treatment charts and includes all data on a specific provider's Patient.
Who can use the closed medical billing system?
The closed medical billing system is highly suitable for stand-alone practices.
ii) Open Medical Billing System
An open medical billing system says much for a synergetic design. Here the complete health data of the Patient gets transferred to more than one practice through Electronic Health Records (EHRs). This billing system offers easy access to information to providers, patients, chief stakeholders, insurance payers, medical billing teams, third-party vendors, and more than one healthcare Organisation.
Who Can Use The Open Medical Billing System?
Larger healthcare Organisations constituting several departments can use an open medical billing system.
iii) Isolated Medical Billing System
Isolated systems are maintained solely by patients, and not any Organisation or provider, through the Personal Health Records (PHR).patient personally maintain these records by directly recording the details at their convenience.
Who Can Use The Isolated Medical Billing System?
The Isolated medical billing system is mainly built for Patient use. Only the Patient can edit, maintain and track this isolated billing system. These records are distinct from EMRs and EHRs and are intended to assist patients in managing their health information.
Services In A Hospital
Understanding Hospital Services Before diving into hospital billing work, it is important to understand the types of services that hospitals typically provide.
Inpatient Care
Inpatient care necessitates an overnight stay in a hospital or medical facility. It can include surgeries, diagnostic tests, and hospital treatments.
Outpatient care
Outpatient care doesn't require an overnight stay in a hospital. It can include visits to the doctor's office, diagnostic tests, and hospital treatments.
Emergency care
Emergency care refers to medical treatment provided in a hospital emergency room. It can include treatment for various medical conditions, from minor injuries to life-threatening illnesses.
How Does Hospital Billing Work - Hospital Billing Cycle
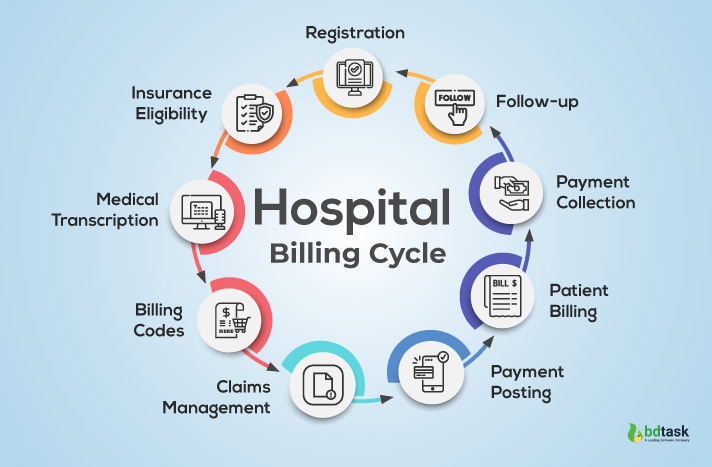
As complex as it is, the hospital billing work can be divided into Nine simple steps. The following are the nine steps of the medical billing process:
1. Patient Registration
How does hospital billing work- The very beginning step is Patient Registration
The starting phase of hospital medical billing work is patient registration. When you arrive at a hospital for medical treatment, you must provide your personal and insurance information to create a medical record and determine how your healthcare services will be billed.
In inpatient registration, the Patient's basic information is collected, like their name, date of birth, insurance information, the reason behind visiting the hospital, etc. Medical billers must be attentive and alert in documenting Patient data to avoid problems.
2. Insurance Eligibility and Verification
Once the Hospital biller has received the Patient's insurance information, they can ascertain which healthcare services are covered by the Patient's insurance plan and which are not. Even regular patients must verify their insurance information and eligibility before every appointment. Insurance information can change anytime, so you must ask patients if their insurance information has changed before every visit.
Insurance coverage differs dramatically between companies, individuals, and plans, so the biller must check each Patient's coverage to assign the bill correctly.
3. Medical Transcription
Medical Transcription refers to transcribing a patient's consultations into a medical record. The purpose of medical Transcription is to convert the Patient's data into written or printed form. The transcriptionist works closely with doctors and patients to turn audio into written notes.
They may also record the conversation between the doctor and Patient to ease making notes and revisit the audio to prevent errors. Clinicians and medical transcription professionals must ensure error-free to facilitate faster bill processing. Providers can also resort to healthcare analytics solutions to improve the medical script.
4. Hospital Billing Codes
The fourth step of How does hospital billing work is Hospital Billing Codes.
The realm of healthcare billing is a convoluted and elaborate system that employs specialised codes to discern the medical services dispensed to patients.
These codes act as a standardised language, facilitating healthcare providers' effective communication with insurance companies and other medical professionals.
(ICD)The system's two most commonly used codes are the International Classification of Diseases codes and the Current Procedural Terminology (CPT) codes.
The ICD codes are an indispensable tool for delineating and identifying medical diagnoses and conditions. They are a uniform approach for healthcare professionals to disseminate information about a patient's medical state. Conversely, the CPT codes are utilised to portray medical procedures and services. They play an effective role in hospital billing work by empowering healthcare providers to bill insurance companies accurately.
Utilising these codes guarantees that medical Billing remains an organised and effective process.
It enables healthcare providers to concentrate on delivering quality care to their patients. It's also guaranteeing that they obtain the compensation they merit for their services.
Despite the complicated nature of hospital billing work, using these codes augments the system's accessibility and comprehensibility for all parties involved.
5. Claims Management
Medical claims management is a complex process that involves several intricate procedures, including
- submission of claims,
- verification of eligibility
- processing of claims
- subsequent follow-up
So let's take a tour of each procedure and how they work.
- Submission of Claims
Healthcare providers can electronically submit claims or through paper forms that comprise comprehensive information, such as Patient demographics, diagnosis codes, and medical procedures.
- Verification of Eligibility
Before processing the claim, health insurance providers verify the Patient's eligibility for coverage by scrutinising their insurance coverage and validating that the services provided are covered under the Patient's plan.
- Processing of Claims
After confirming the claim's validity, the health insurance provider processes the claim and determines the reimbursement amount based on the Patient's plan coverage.
- Follow-up In case
If the claim is refused or rejected, healthcare providers can contact the insurance provider to settle any problems and resubmit the claim if necessary.
6. Payment posting
How does hospital billing work- coming up? Payment posting
Payment posting refers to viewing the payments and the financial picture of the medical practice.
After the insurance company approves the claim, payment will be sent to the hospital. Subsequently, the payment will be entered into the Patient's account, and the balance will be adjusted accordingly.
7. Patient Billing
If there is still an outstanding balance after insurance payment, the hospital will invoice the Patient for the remaining amount. The statement sent to the Patient will include a summary of the charges, insurance payments, and the outstanding balance.
Patient billing is kind of lengthy process. From information to the transaction process is kind of slow. All the retail stores use a simple POS system then why not a hospital?
When a hospital connects a POS system, it can also deliver insight into the entire chain of medical billing work.
So why hospital POS system is important
A point-of-sale system is no ordinary cash register
- Tracking and storing your transactions.
- Ability to keep records of daily transactions accurately.
- Tracking your inventory 24/7
- Automate a lot of the processes
- Simplify and accurate the hospital billing work.
- Record all the patient billing data.
Overall a hospital POS system helps to make all hospital billing work 10 times faster than usual.
Make your hospital more efficient through a POS system
The beauty of real-time and the hospital POS system is that it collects all the data and has all that information at your fingertips. It is the ability to see gaps and identify ways to eliminate wasteful spending; this is probably the most useful feature.
8. Payment collection
Upon receipt of the bill, the Patient is responsible for paying the remaining balance. The hospital may offer payment options or financial assistance programs to assist patients in paying their bills.
9. Follow-up
The final step of How does hospital billing work is Hospital Billing Codes.
The final stage of the hospital billing process is a follow-up, which involves reaching out to the Patient to ensure that the bill has been paid in full and to address any concerns or questions they may have.
Last of all but not the list, If you do not have health insurance or if your insurance does not cover the full cost of your medical treatment, the hospital will typically offer several payment options. These options can include payment plans, financial assistance programs, and discounts for paying in full at the time of service.
Why Is Hospital Billing Complicated?
Medical bills contain many codes and descriptions that may be hard to understand. That's because medical billing systems are primarily set up to facilitate payment from insurance companies and government programs such as Medicare and Medicaid. These payers require bills to be submitted and formatted using specific diagnosis, treatment, and supply codes, or the bills won't get paid.
Common Medical Billing Errors
Medical billing errors can have significant consequences for healthcare providers, including financial losses, delayed payments, and Patient dissatisfaction.
Hospital Billing errors result in Billions of dollars.
Types Of Medical Billing Errors
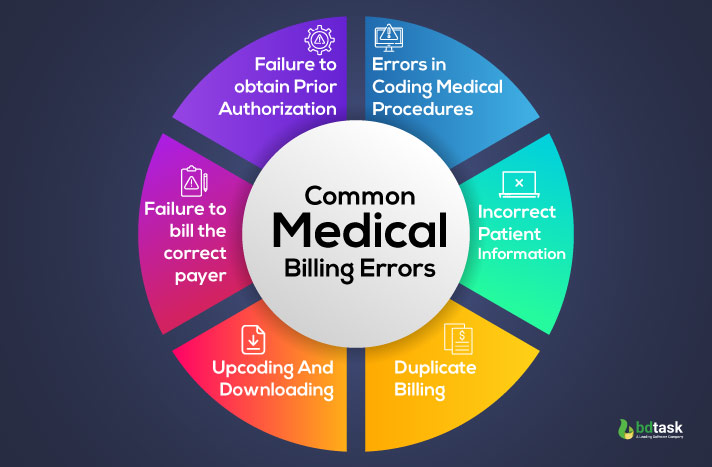
1. Errors in coding medical procedures
One of the most common medical billing errors is incorrect coding of medical procedures. It can result in overbilling or underbilling for services rendered, leading to delayed payments.
2. Incorrect patient information
Incorrect patient information can include misspelt names, incorrect insurance, or outdated contact information. Incorrect patient information, something like
- Incorrect spelling of the Patient's name
- Incorrect date of birth
- Mistakes while filling in the sex of the Patient
- Insurance policy number
- The insurance payer's name
- The Patient's relationship
3. Duplicate Billing
What are the most common denials you can see in the hospital?
More or less, it's a duplicate billing problem.
According to Health Payer Intelligence,
46% of medical fraud cases occur due to either Fraudulent provider billing or Double Billing
These claim errors happen when a healthcare Organisation
- Bills for the same patient procedure, treatment, or testing on multiple occasions.
- Make Billing for the wrong patient service.
- Bills for patient services that were never performed.
- Charges many times for the same medicine.
4. Upcoding And Downloading
Upcoding occurs when a provider bills for a more expensive service than what was provided. In contrast, Downcoding occurs when a provider bills for a less expensive service than what was provided. All those practices are legally called fraudulent.
5. Failure to bill the correct payer
Billing errors can also occur when providers bill the wrong payer, such as billing a patient's primary insurance when the service should have been billed to their secondary insurance.
6. Failure to obtain prior authorisation
Some medical services require prior authorization from insurance companies before being billed. Failure to obtain prior authorization can result in denied claims and delayed payments.
Causes of Medical Billing Errors
1. Lack of training or knowledge in medical billing and coding
Lack of training is one of the main issues creating medical errors. Sometimes wrong coding and outdated coding is the reason for billing errors. What do you think when your medical staff does not have enough knowledge? Will they give the best treatment? Of course not. And the result is billing errors.
2. Human Error
Billing errors can also occur due to human error, such as types or mistakes in data entry. Human errors form a considerable portion of preventable mishaps in hospitals. Even the most competent hospital are not immune to it. Errors in the perioperative period can often have grave consequences.
3. Danger of Poor communication
Communication in healthcare may appear unimportant, but it can be a big deal. Poor communication can cost to poor outcomes for patients.
Poor communication occurs between healthcare providers and billing staff. Effective communication between healthcare providers and billing staff is essential to ensure accurate Billing.
Failure to communicate effectively can result in billing errors.
4. Outdated Or Inaccurate Technology
Outdated or inaccurate technology can also lead to billing errors. Providers should invest in accurate and up-to-date billing software to minimise the risk of errors.
Let's Meet The Consequences
1. Financial loss
Medical billing errors can result in significant financial losses for healthcare providers. It can include lost revenue due to denied claims and increased administrative costs associated with correcting billing errors. It's also very bad for the hospital revenue cycle.
2. Delayed payments
Billing errors can also result in delayed payments, which can cause cash flow problems and reduce hospital billing work for healthcare providers.
3. Patient Dissatisfaction
Patients may also be dissatisfied with billing errors, as they can result in confusion and frustration over bills and insurance coverage. It can be hard to explain to a patient why a claim has been denied or is late being paid. The Patient might have to pay unplanned out-of-pocket medical expenses when their ability to earn money has been diminished due to illness or disability.
4. Increased administrative costs
Billing errors can also increase administrative costs, as staff may need additional time correcting billing errors. Many hospitals still rely on manual billing processes, which are prone to errors and require significant administrative work. Hospital billing work in the same way in many countries. Another reason for administrative costs is Hospital staff may spend a significant amount of time verifying insurance coverage and eligibility. Duplication of effort can lead to unnecessary costs.
Tips For Avoiding Medical Billing Errors
1. Invest in training and education for billing and coding staff
Healthcare providers should ensure that their billing and coding staff receive proper education and training to minimise the risk of errors. Proper training and proper Billing and coding reduce medical billing errors.
2. Implement efficient billing processes
Providers should implement efficient billing processes, such as electronic Billing and automated claim submission, to minimise the cost and gain some revenue.
3. Use Accurate And Up-To-Date Technology

Providers should use accurate and up-to-date billing software to minimise the risk of errors.
Billing systems in a hospital or medical Billing software automate the manual task of Billing to ensure faster payment. This benefits provider by making the processing faster, improving workflow, and tracking patient information. Implementing a billing system in hospitals will boost its revenue too.
Hospital Automanager is the best choice for any hospital. All facilities are in one simple, flexible, responsive software. You can get proper control of your hospital work. When automation software controls all the work, it will help you to reduce all the errors of medical Billing that you face earlier. More or less; you will get a proper system that can handle all the pressure.
let's explore some of the best Exotic features of Hospital Automanager:
- Creates separate interfaces for (doctors, nurses, and patients)
- Administration portal
- Billing management system
- Cloud-based technology
- Patient management system
- Bed management system
- Online appointment system
- Integrates HR management system
- OPD and IPD management systems
- Employee management system
- Alert system facilities
- Account management system
- Payment management system
- Report system
Believe it or not, using hospital management software will make life much easier for any medical provider—something like an Aladin Chirag and a game changer for any hospital. Good hospital management software helps any hospital reduce billing errors and human Errors and reduces administrative costs also. When all the work goes smoothly, the Patient gets all the requested treatment. At the end of the day hospital also gets some revenue. One of the main things is that it also gains the hospital brand value, and when a patient gives you a good review, it will help you get more patients.
The Bottom Line
Now you know how hospital billing works. Hospital billing is a complex process that involves multiple parties and steps. Patients should understand their insurance coverage and benefits and carefully review their medical bills to avoid unnecessary charges. The simple and cost-effective solution is proper hospital management software to get more positive results. Choose hospital Automanageer as your partner and get ready to improve your revenue cycle management and earn maximum profits. Patients receive the necessary medical treatment without incurring undue financial burdens.









